Findings
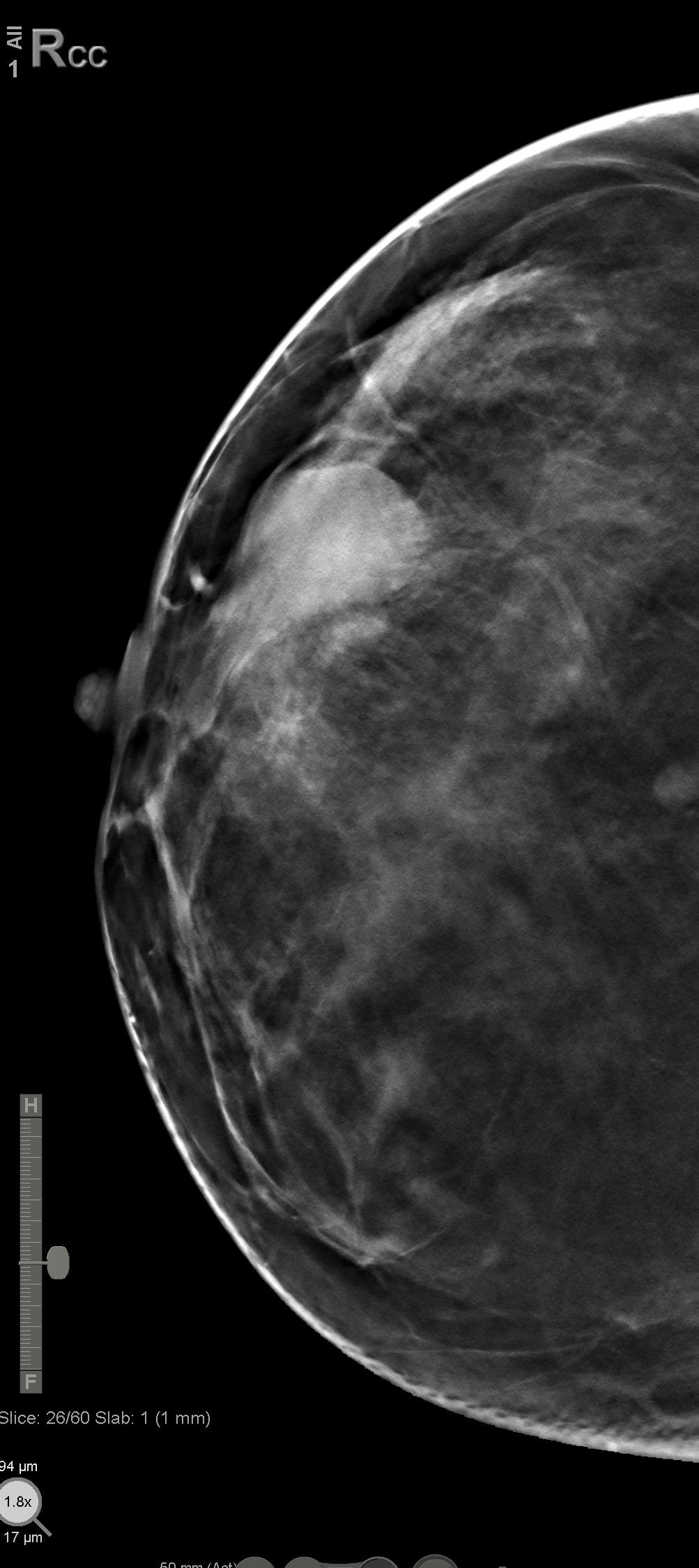
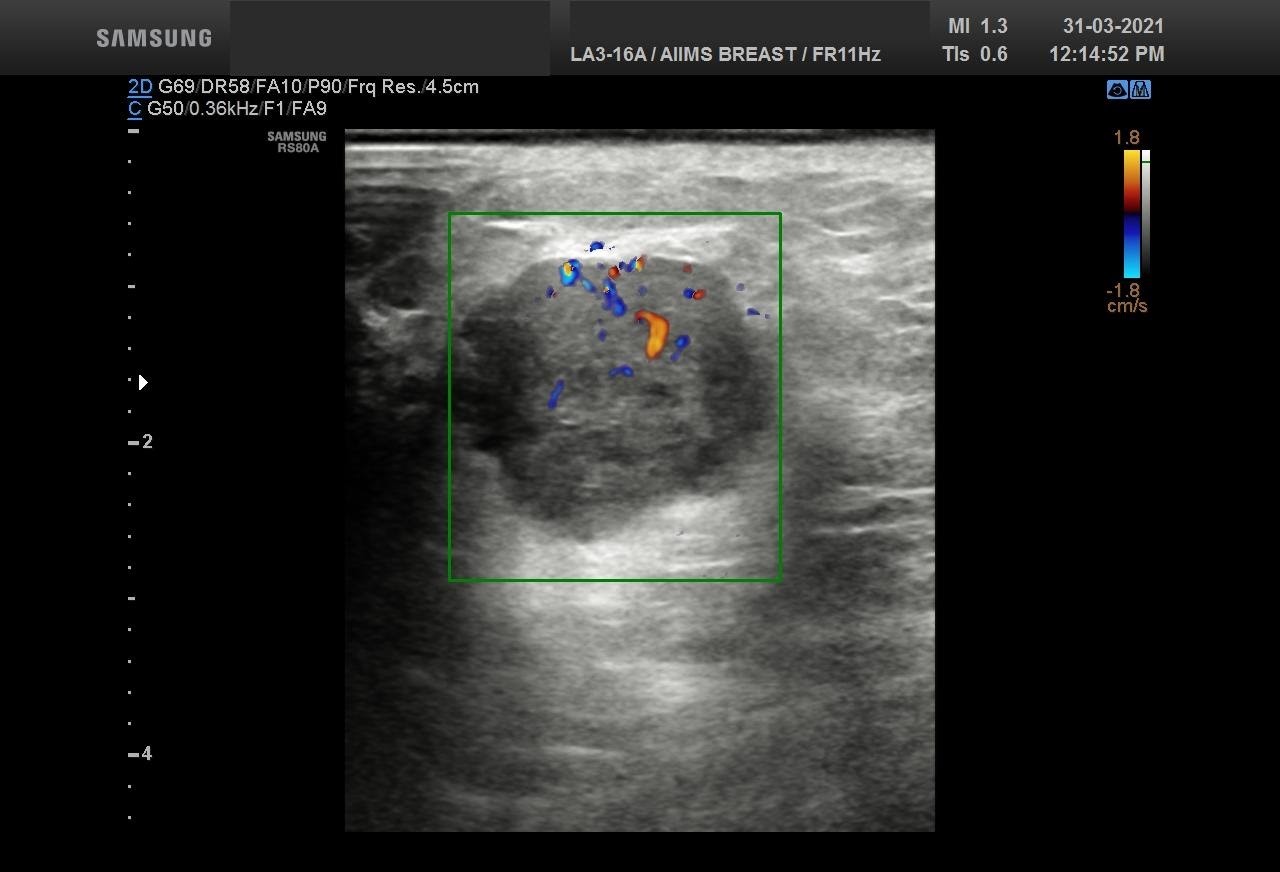
Bilateral Digital mammography , Craniocaudal (CC) and Mediolateral oblique (MLO) view with tomosynthesis images revealed a round shaped, equal density mass with indistinct margin in lower outer quadrant. No suspicious microcalcifications was seen. No significant axillary lymph nodes were present. A high resolution ultrasound of the right breast showed a round shaped, heterogeneously hypoechoic mass with irregular margin, small cystic spaces within and posterior acoustic enhancement, measuring about 1.6x1.9x1.5cm at 7 O’clock position. Mild internal vascularity was noted on colour doppler images. Right axilla showed suspicious lymph nodes with loss of fatty hilum and thickened cortex.
Answer
Although the mass has few benign features like round shape and posterior enhancement, presence of irregular margin and axillary nodes with thickened cortex and loss of fatty hilum points towards the suspicious nature of the mass. So, the mass was classified as BIRADS category 4b lesion. Ultrasound guided biopsy of the mass was suggestive of invasive breast carcinoma with possibility of medullary carcinoma. IHC study showed tumor to be Positive for PR and negative for ER and HER2neu receptors. Patient underwent Breast conserving surgery with right axillary lymph node dissection and final histopathological report was Invasive carcinoma with medullary features. Axillary lymph nodes were involved by the tumor.
Discussion
Medullary carcinoma of breast (MCB) is a very rare subtype of breast cancer accounting for 1 to 7% of all breast cancers. They tend to occur in younger age group as compared to other breast cancers but have a better survival rate than the common infiltrating ductal carcinomas . The mean age of presentation is 45 to 54 years with about 10 % of patients being in age group under 35 years. It is common in women with BRACA 1 mutation. It is unicentric in most of the patients whereas bilateral carcinomas has an incidence ranging from 3% to 18%. Most of the patients present with a palpable mass, usually in upper outer quadrant. On mammogram it is typically seen as a circular or oval shaped mass with circumscribed or indistinct margin. Microcalcification is usually not seen. On ultrasound also it is usually seen as a circumscribed round or lobulated mass with homogenous or heterogenous hypoechoic echotexture. Posterior enhancement may be present. The most common MRI findings are oval or lobular shaped masses with circumscribed margin. It usually shows homogenous or heterogenous enhancement in early phase with rim enhancement in delayed phase. On dynamic studies, all medullary tumours present a rapid initial rise on time-intensity curve with either a plateau (Type II curve)or a wash-out kinetics (type III curves). Thus MCB has pseudo-benign imaging appearances and in younger age can be mistaken clinically as well as radiologically as fibroadenoma leading to delay in diagnosis . Cho et al suggested that in a circumscribed mass on sonogram, the presence of taller than wide shape, a focally thick wall, an internal irregular cystic space and axillary lymph node enlargement should prompt radiologist to consider medullary carcinoma as a differential diagnosis in addition to fibroadenoma. On MRI in morphologically benign lesion, the presence of diffusion restriction, peripheral rim enhancement and Type II or III kinetic curve in a dynamic contrast enhanced study would suggest a malignant lesion and possibility of medullary carcinoma should also be considered. Histological diagnosis of typical Medullary carcinoma is made when the morphologic criterias as defined by the WHO are met which include syncytial growth pattern, no glandular or tubular structures, diffuse lymphoplasmacytic infiltrate , moderate to marked nuclear pleomorphism and complete histologic circumscription. The terms ''atypical medullary carcinoma'' and ''carcinoma with medullary features'' have been proposed for tumors that do not fulfill all these criteria. According to 2012 WHO recommendation now all classic medullary carcinoma, atypical medullary carcinoma, and invasive carcinoma of no special type with medullary features are grouped within the category of “carcinomas with medullary features”. Immunohistochemical results have shown that MCB are most often negative for estrogen (ER), progesterone (PR), and human epidermal growth factor receptor 2 (HER2)2 i.e. Triple negative tumor . Treatment is same as that of Infiltrating ductal carcinoma and it carries a favourable prognosis compared with infiltrating ductal carcinoma. Two most important prognostic factors are size of the tumor and lymph nodal status and thus patients with tumor size >3cm and metastatic nodes have poorer prognosis. The overall 10 year survival rate is 74% and over 90% in patients with negative lymph nodes.
Reference
1. Park I, Kim J, Kim M, et al. Comparison of the characteristics of medullary breast carcinoma and invasive ductal carcinoma. J Breast Cancer. 2013;16(4):417-425. 2. Jeong SJ, Lim HS, Lee JS, Park MH, Yoon JH, Park JG, Kang HK. Medullary carcinoma of the breast: MRI findings. AJR Am J Roentgenol. 2012 May;198(5):W482-7. 3. Pintican R, Duma, M, Chiorean, A, Fetica, B, Badan, M et al., Mucinous versus medullary breast carcinoma: mammography, ultrasound, and MRI findings, Clinical Radiology, https://doi.org/10.1016/j.crad.2019.12.024 4. Cho, Nariya & Oh, Ki & Lee, Sung. (2002). Medullary Carcinoma of the Breast: Sonographic Features Distinguishing It from Fibroadenoma. Journal of Medical Ultrasound. 10. 191-196. 10.1016/S0929-6441(09)60035-7.