
















Dr. Janaki P Dharmarajan
Amrita Institute of Medical Sciences
29 year old uniparous lady from Middle East presented with right breast lump and yellowish nipple discharge of three weeks duration. FNAC from elsewhere was benign. Clinically firm lump in right lateral quadrant with mild skin induration. Evaluated with baseline mammography, ultrasound and MRI followed by core biopsy and finally excision biopsy.
Post traumatic fat necrosis
Findings
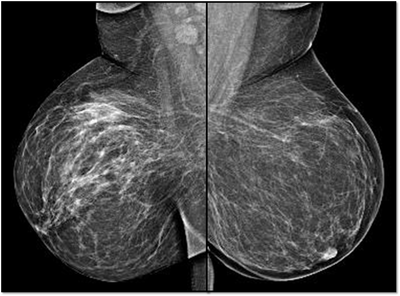
MG: Right breast shows focal asymmetric density in lateral quadrant extending for an area of 12.4 x 6.5 cm with no associated discrete mass or suspicious calcifications. Correlative ultrasound showed a heterogeneous area with echogenic vascular surrounding parenchyma in lateral quadrant with no discrete solid masses. MRI breast was performed on day 14 of LMP. Right breast shows an area predominantly consisting of fat in lateral quadrant extending for an area of 1.2×5.5x 8.9 cm along its maximum AP, ML and CC dimensions. This area is bright on fat suppressed T2 sequences and shows significant restriction on diffusion weighted sequences. There is rapid and progressive non mass enhancement in the above area extending anteriorly in to the nipple and posteriorly into the pectoralis major muscle. Two large and tortuous feeding vessels are seen to arise from the subclavian and axillary arteries respectively. Right breast shows predominantly fat containing mass showing abnormal enhancement described. The possibilities include vascular neoplasm or remotely fat necrosis. Ultrasound guided core biopsy was Suggestive of an inflammatory lesion, possibly fat necrosis. However enlarged and tortuous feeding arteries to the vascular mass was worrisome and we recommended an excision biopsy correlation. Excision biopsy showed “Multiple patchy areas of dense inflammatory infiltration in a background of fat necrosis”.
Discussion
This lady had h/o accidental injury to breast by way of her child’s head butting. First case of Traumatic fat necrosis of female breast was reported in 1920 by Lee and Adair. Clinically fat necrosis can result from accidental trauma, but more often it is iatrogenic and commonly seen after surgery or radiation therapy. Aqel et al demonstrated that .97% of symptomatic fat necrosis patients present with palpable abnormalities. Palpable breast abnormalities associated with fat necrosis may enlarge, remain unchanged, regress or resolve (1). Fat necrosis is a disintegration of fat cells with the associated tissue reactions of new connective tissue formation and the production of foreign body giant cells. In early stage, haemorrhage occurs in fat. Over several weeks, cystic degeneration sets in along with calcifications in cyst walls. In the intermediate stage of fat necrosis, there is infiltration of histiocytes and multinucleated giant cells. In the late stage of fat necrosis, usually hemosiderin deposition and the development of fibrosis. The reactive inflammatory components are replaced by fibrosis leading to scar formation. Sometimes, fibrosis and calcifications are the only sequelae of fat necrosis. Thus,the varied appearances of fat necrosis on imaging studies are attributed to various amounts of histiocytic infiltration, hemorrhage, fibrosis, and calcification. MG features : Fat necrosis can present as lipid cysts, coarse calcifications, focal asymmetries, microcalcifications, or spiculated masses. Mammographic appearance reflects the amount of fibrosis. Ultrasound features: Fat necrosis can present as a solid mass, a complex mass with mural nodules, a complex mass with echogenic bands, an anechoic mass with posterior acoustic enhancement, an anechoic mass with shadowing or an isoechoic mass. The margins may be circumscribed, indistinct or spiculated. A mass with echogenic internal bands that shift in orientation with changes in patient position has been described as a specific sonographic indicator of fat necrosis. MRI features: Fat necrosis is a great mimic of malignancy on MRI based on morphology and enhancement kinetics. Necrotic fat shows low signal on T1 due to its haemorrhagic and inflammatory content. Fibrosis is seen as architectural distortion with or without any associated spiculated masses. Amount of enhancement depends on the intensity of inflammatory processes. Needle biopsy is indicated if diagnosis of fat necrosis is not certain.
Together we are making a difference- and, you can too..