Findings
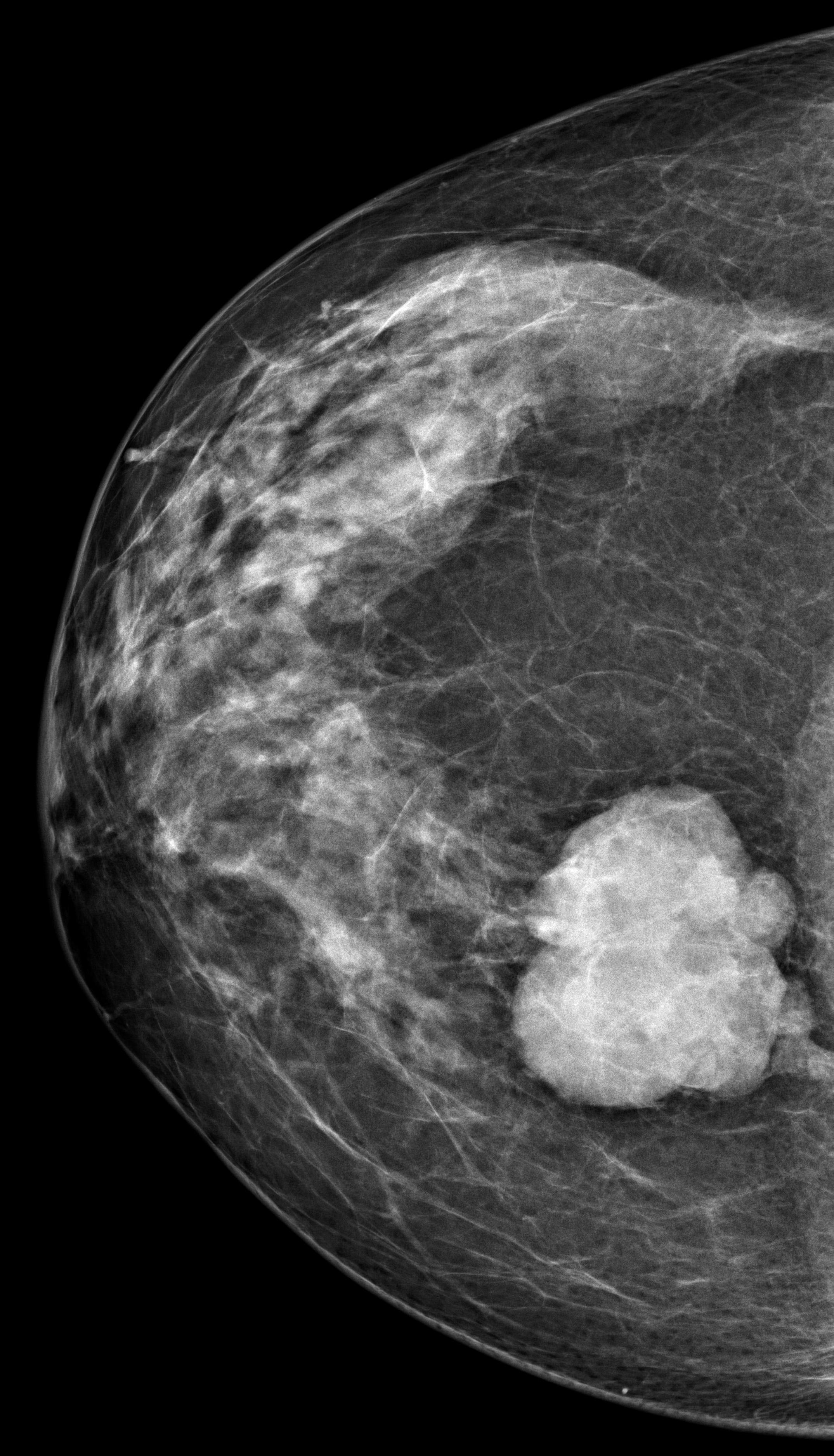
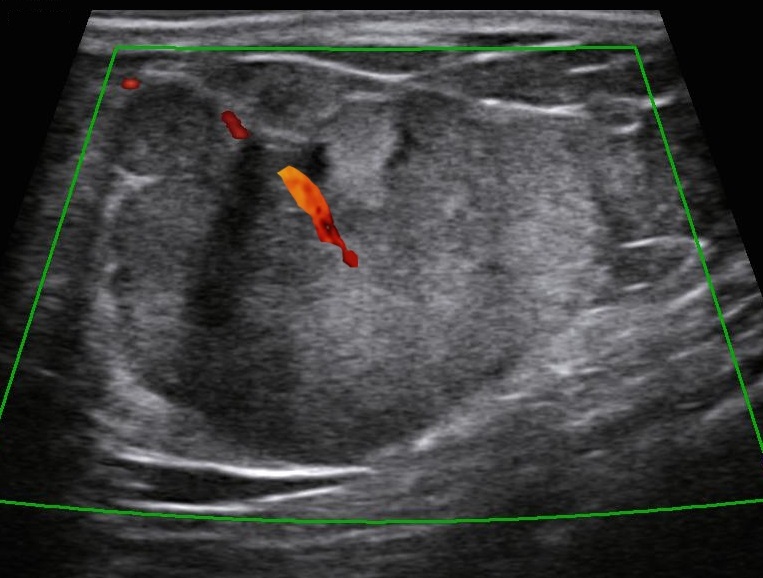
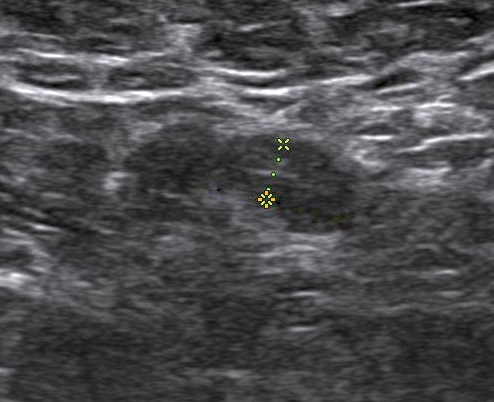
Bilateral digital mammography with tomosynthesis and ultrasonography was done. Mammography revealed a high-density irregular mass with multilobulated margins in the upper and outer quadrant of the left breast. The mass was located eccentric to the nipple. No associated calcifications were seen.No axillary lymphadenopathy. Ultrasonography revealed a hypoechoic irregular mass with multilobulated margins at 2 o clock position in the left breast. Color doppler revealed minimal peripheral vascularity. Arfi elastography revealed the mass to be hard. A BI-RADS assessment category of 4C was given with a recommendation for a core needle biopsy. Histopathology Invasive ductal carcinoma .IHC -ER 95 %,PR-95% ,HER 2 -Negative and KI -67-20%. PET CT revealed an FDG avid lesion in the upper outer quadrant of the left breast with no axillary or distant metastases.
Answer
Male breast cancer
Discussion
Introduction Men can present with palpable lumps in the breast the most common cause being gynecomastia. Malignant lesions in the breast are rare and account for less than 1% of the breast lesions (1). The common clinical presentations are a palpable hard lump, bloody nipple discharge, retraction of the nipple, and enlarged axillary lymph nodes. The imaging modality of choice for the male breast is bilateral mammography followed by high-resolution ultrasound for in-breast staging as well as for core biopsy guidance. The male breast does not contain the terminal ductal lobular units into (TDLU), and hence lesions originating from the lobules for example cysts, fibroadenomas, and lobular cancers are extremely rare and therefore all masses with circumscribed margins in a male breast need to be viewed with suspicion and be evaluated. Male breast cancers account for 0.7% of all breast cancer and 0.17% of all cancers in men) and are exceedingly rare. Risk factors Genetic and chromosomal conditions like BRCA2 mutation and Klinefelter syndrome, Jewish, Egyptian, or West African descent, advanced age, irradiation of chest wall in a young age and prostatic cancer treatment with exogenous Estrogen, liver parenchymal disease, and other diseases associated with increased estrogen levels and androgen deficiency due to testicular dysfunction. A family history of breast cancer in the first-degree relative increases the risk by 2-4-fold. 60%–76% of Male Breast cancer is caused by BRCA2 mutations which are much more common than BRCA1. Gynaecomastia is not a risk for breast cancer. Clinical presentation: Male breast cancers can present as a painless hard mass located in the sub areola region and eccentric to the nipple, nipple discharge, nipple retraction, skin ulceration, or axillary lymphadenopathy. The commonest histological variant seen in over 85% is invasive ductal carcinoma of the “not otherwise specified” with luminal A and B subtypes being the major types . followed by ductal carcinoma in situ and uncommonly invasive lobular carcinoma. Imaging: Mammography: Male breast cancer presents mammographically as a high-density irregular mass with spiculated, lobulated, or microlobulated margins. Male breast cancer arises from the central ducts and hence mostly are retro areolar in location. The appearance of a discrete mass, eccentric location, and secondary features allow distinction from allows distinction from gynecomastia. Microcalcification is less commonly seen in males and is seen associated with the infrequent occurrence of ductal carcinoma in situ. Enlarged lymphnodes may also be seen in the axilla and sometimes maybe the presenting feature of male breast cancer. Secondary features like nipple retraction, skin thickening, and increased trabeculation may be seen indicating advanced disease and have a poorer prognosis. As the size of the male breast is smaller, secondary features are seen more frequently in men and are associated with a smaller size of tumor than in women. Ultrasound: The ultrasound features of male breast cancer and female breast cancer are similar. The masses appear hypoechoic irregular, with a non-parallel orientation with no posterior features. Colour Doppler may reveal increased vascularity. On elastography, the masses appear hard. Ultrasound helps in evaluating the relationship of the nipple with the mass. In malignant lesions, it is subareolar and eccentric and in gynecomastia, it is subareolar and central. In patients presenting with nipple discharge ultrasound helps in demonstrating nipple involvement by the tumor and intraductal extension. Skin thickening and lymphoedema of the subcutaneous planes and enlarged axillary lymph nodes with thickened cortex are secondary changes and are well demonstrated on ultrasound. Image-guided biopsies and axillary lymph node sampling are always done ultrasound-guided due to the small size of the male breast. MRI: MRI is helpful in evaluating the involvement of the chest wall by the mass as well as axillary staging. Management and surveillance recommendations Breast cancer trials have included few men and therefore recommendations regarding management of breast cancer in men are extrapolated from clinical trials from breast cancer in women. Historically, men undergo mastectomy for breast cancer more often than breast conservation surgery, however, data indicates that breast conservation in men is associated with equivalent outcomes to mastectomy. As in women, SNLB should be performed in all node-negative patients with breast cancer. Options for adjuvant endocrine therapy for men with breast cancer include tamoxifen for 5-10 years. If tamoxifen is contraindicated then a GnRH analog plus an aromatase inhibitor is given. The NCCN panel recommends consideration of Genetic testing for all men with breast cancer. Management of systemic therapy for advanced disease is similar to breast cancer in women. Routine mammography is not required for patients with early breast cancer on surveillance following treatment although the contralateral breast may undergo routine screening. Bone density is recommended before and after therapy for patients who receive GnRH analog therapy,
Reference
1. Chen L, Chantra PK, Larsen LH, et al. Imaging characteristics of malignant lesions of the male breast. Radiographics. 2006;26(4):993-1006. 2.Rizzolo P, Silvestri V, Tommasi S, et al. Male breast cancer: genetics, epigenetics, and ethical aspects. Ann Oncol. 2013;24 Suppl 8:viii75-viii82. 3. Mathew J, Perkins GH, Stephens T, Middleton LP, Yang WT. Primary breast cancer in men: clinical, imaging, and pathologic findings in 57 patients. AJR Am J Roentgenol. 2008;191(6):1631-1639. doi:10.2214/AJR.08.1076 4. Mainiero MB, Lourenco AP, Barke LD, et al. ACR Appropriateness Criteria Evaluation of the Symptomatic Male Breast. J Am Coll Radiol. 2015;12(7):678-682.